Intense Pulse Light Therapy (IPL)
Eye Doctor MD, P.C. is the local eye center for the communities of Glen Allen, Richmond, and the surrounding areas. Our board-certified ophthalmologist and cornea specialist, Dr. Shilpi Pradhan, provides our patients with personalized treatments for conditions such as glaucoma, cataracts, dry eye disease, and more. Our eye center is equipped with state-of-the-art treatment technology, including the IPL.

IPL Now Available At Eye Doctor MD, P.C.
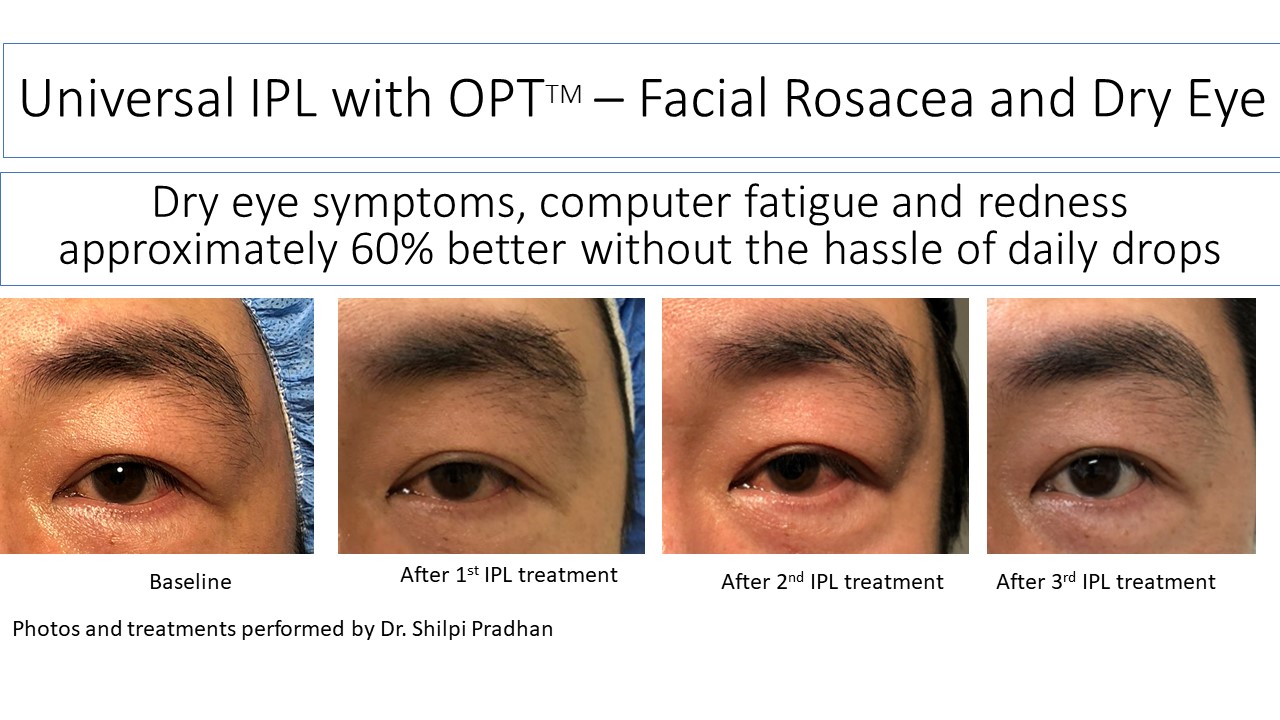
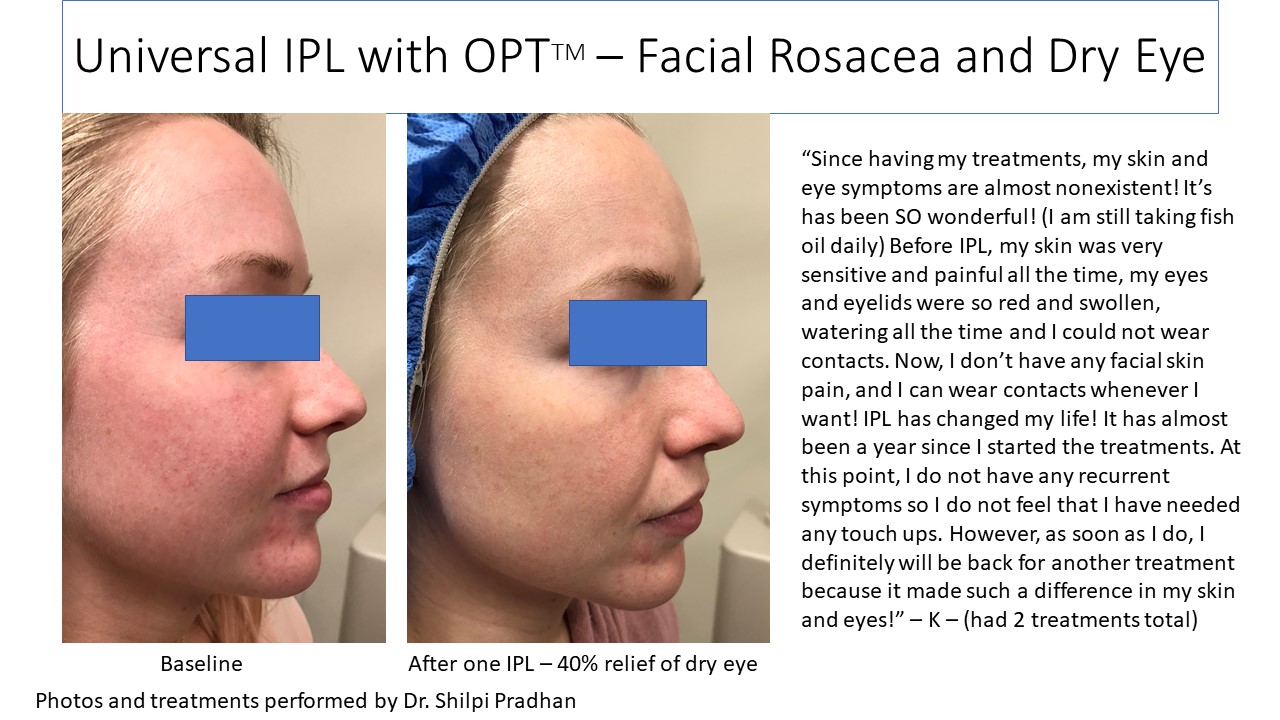
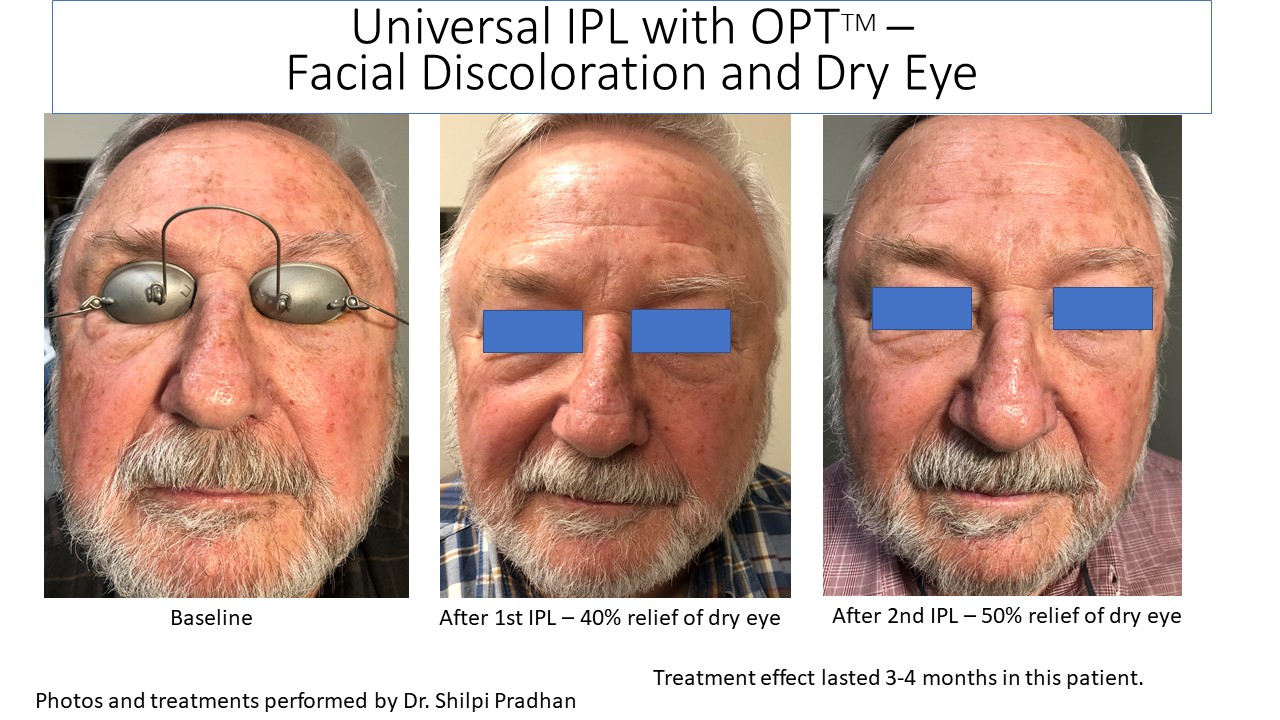
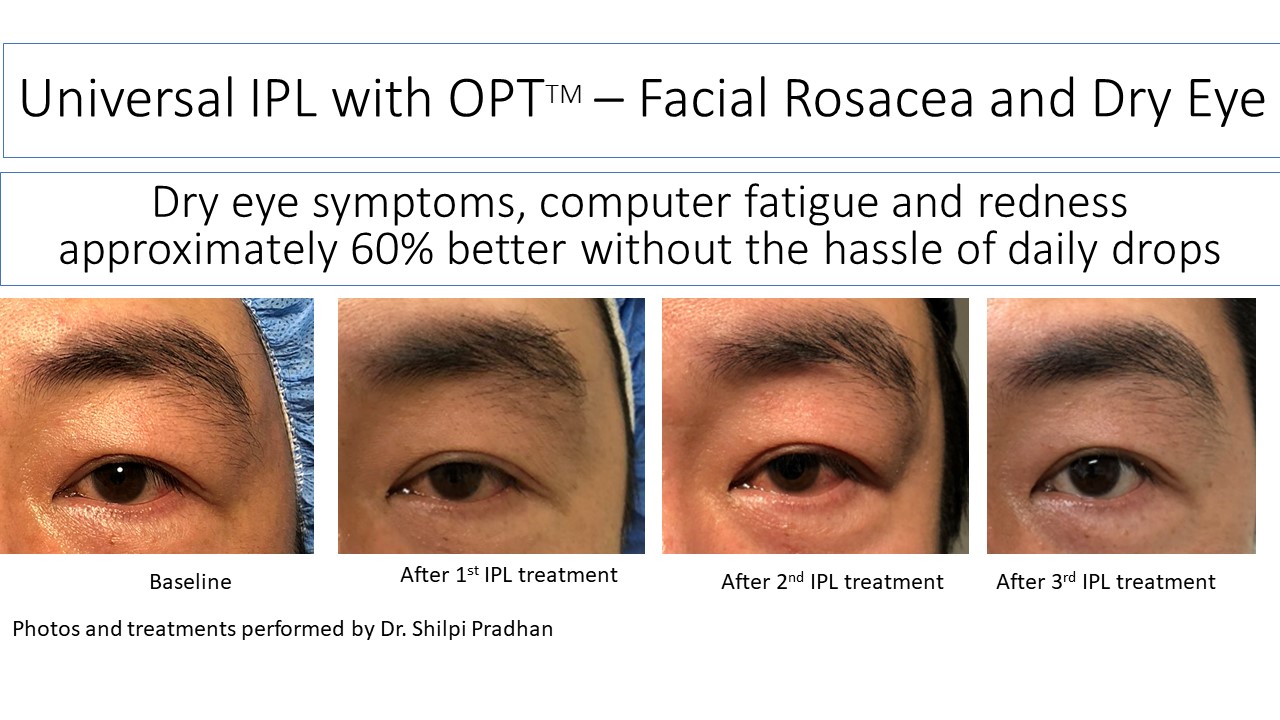
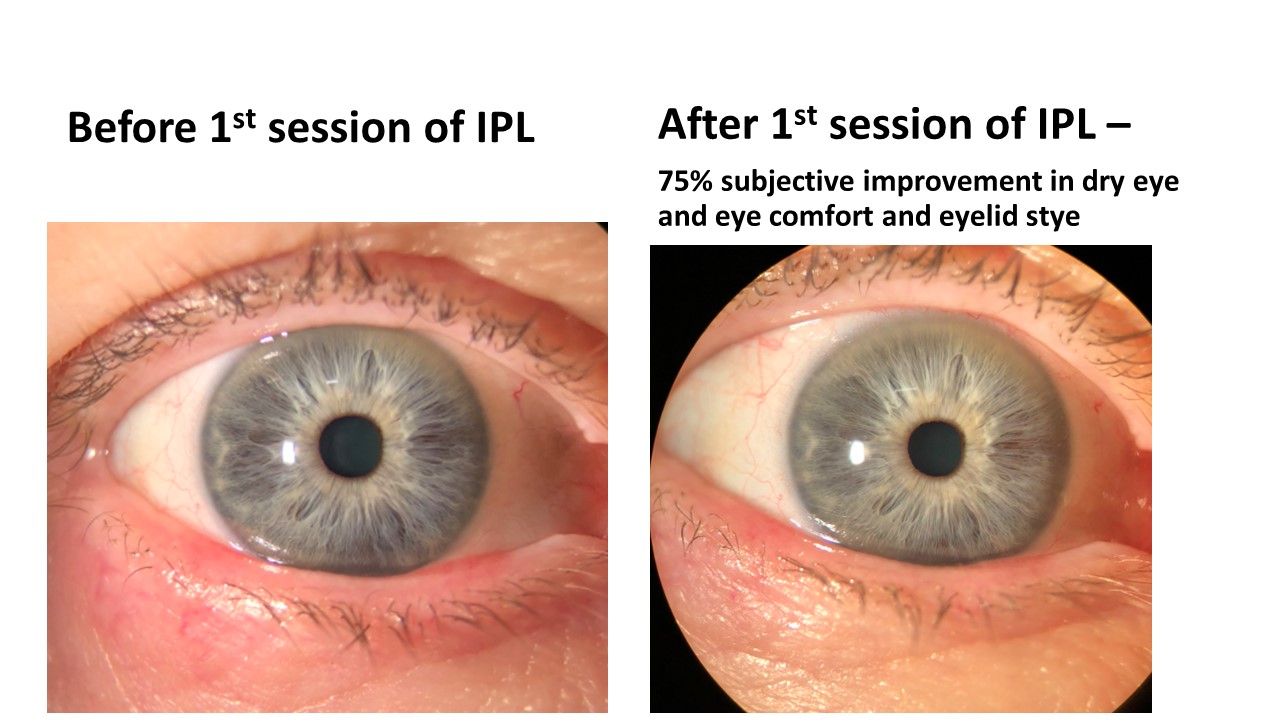
We are excited to present the IPL (Intense Pulse Light), known to help with rosacea, skin discoloration and now dry eye disease. The IPL helps photo-rejuvenate the skin and help the function of the meibomian glands of the eyelids, helping improve the quality of the meibum produced. IPL treatment is not covered by insurance. We are pleased to offer it for dry eye disease (DED protocol) or full face (rosacea protocol including DED). Please contact us for pricing. You may need multiple treatments (4-6 total) to achieve optimal results and then maintenance treatments once yearly with an eye doctor.
What is IPL?
IPL stands for Intense Pulse Light. It is a treatment that has been around for decades in the world of dermatology to treat rosacea. Dr. Toyos, a specialist in ophthalmology, discovered that his dry eye patients were also improving when they had IPL for their face and over the years, has developed a dry eye disease protocol to help patients with dry eye disease (DED) with a component of meibomian gland dysfunction (MGD).
How Does IPL Work?
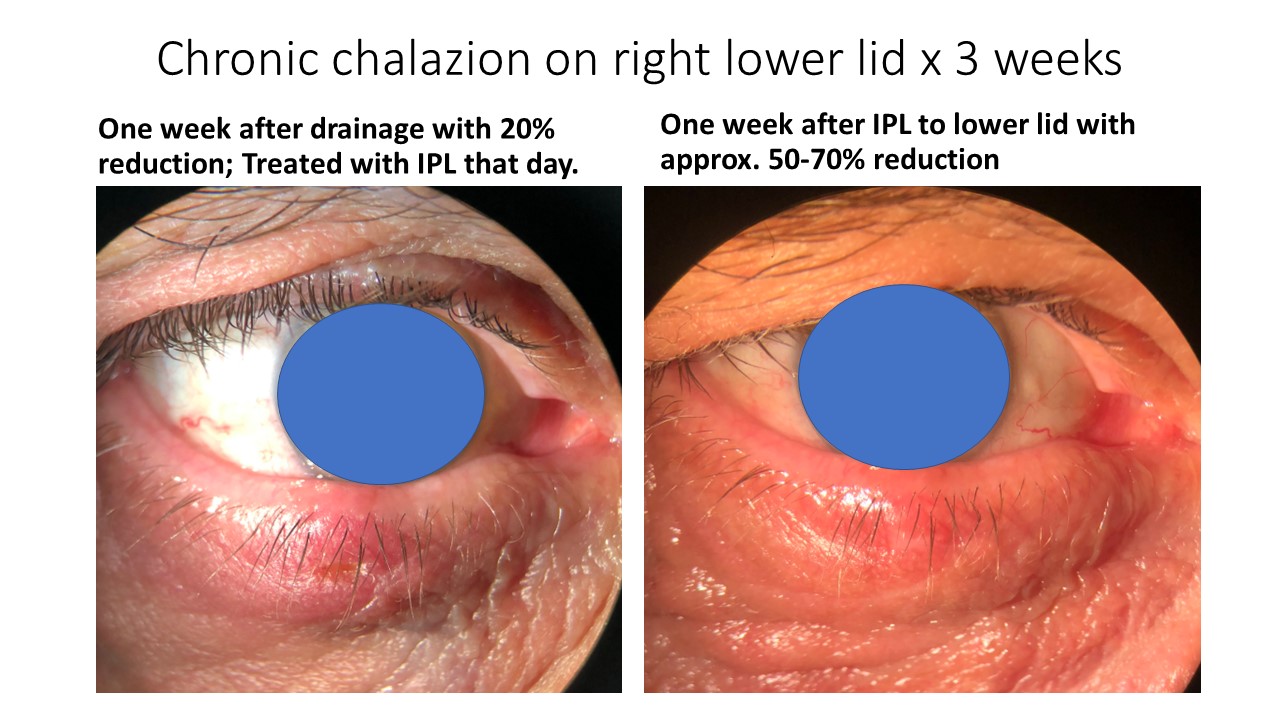
The meibomian glands are located in your eyelids and produce the meibum (or the oily layer) of the tear film that prevent the tears from evaporating. MGD occurs when the meibomian glands are obstructed or inflamed. In patients with either facial or ocular rosacea, the eyelids have abnormal dilated blood vessels (telangiectasia) that bring more inflammation to the surface of the eyelid and can cause dysfunction of the meibomian glands. IPL causes photocoagulation of those abnormal blood vessels and photorejuvenation of the skin cells. IPL also stimulates the stem cells of the meibomian glands to help them make better oil. It also causes dilation of the meibomian glands and liquification of the obstructed meibum. After the IPL treatment, Dr. Pradhan follows the DED protocol to manually express the meibomian glands or in combination with the Lipiflow treatment. Patients generally feel some relief even after one session (up to 89% of patients had improvements in symptoms)1.
Tell Me More About IPL
Dr. Pradhan is pleased to offer the Lumenis M22 for IPL given the safety features with contact-cooling which make it safe and comfortable for dry eye treatment. Dr. Pradhan was one of the first doctors in the Ricmond area to offer IPL for dry eye disease since December 2017 and has extensive experience.
It also has different filters which allow it to be used for different purposes including the dry eye disease protocol, full-face rosacea as well as skin discoloration. The dry eye disease protocol involves treatment from one side of the face to the other including the lower lids as well as Meibomian gland expression afterwards. The upper lids benefit from the treatment although they are not treated directly with the IPL (in the original studies however Dr. Pradhan treats all lids directly) and all four lids are expressed after the treatment. IPL treatment at our local eye center generally takes approximately 15 minutes. Your eyes are covered with laser grade metal shields the entire time to prevent any damage directly to your eyes. The IPL also has the ability to kill bacteria and even kill demodex and has been shown to help blepharitis as well. If you have blepharitis, it will be important to remove the crusting with the BlephEx procedure prior to treatment with the IPL. Read an updated blog post about the science of IPL!
How Many Treatments Do I Need?
The studied protocol for dry eye disease with the IPL involves 4 initial treatments approximately 3-5 weeks apart and then once annually, all with a professional ophthalmologist, like Dr. Pradhan.
How Is The IPL Different Than The Lipiflow?
Dr. Pradhan is leading the way for dry eye treatment options available by offering IPL for dry eye disease. Both the IPL and the Lipiflow treat the underlying cause of evaporative dry eye disease with meibomian gland dysfunction. The IPL works on the inflammatory blood vessels and is only safe for certain skin types and works best in patients with ocular or facial rosacea. The Lipiflow heats, unclogs and expresses the obstruction of the meibomian glands and can be used in all skin colors/types. With a dry eye evaluation, Dr. Pradhan can tell you which one is better for you or whether a combination treatment would produce the best results.
Are There Any Contraindications For IPL Treatment Of Dry Eye?
- No sun exposure or tanning beds or tanning cream for 3-4 (minimum 2) weeks prior to treatment; no harsh scrubs, acids, benzoyl peroxide, Retin-A
- No use of isotretinoin (Accutane) within the last year
- Pregnant, postpartum or nursing
- History of cancer in the area of treatment
- Active cold sores or herpes simplex or herpes zoster virus
- History of keloids
- History of metal plates, rods or screws in the area
- Use of any photosensitive medications or herbal supplements
- Includes use of antibiotics
- Psoriasis, vitiligo or warts, lupus or connective tissue disorder
- Avoid Botox and dermal fillers for 1 week prior to treatment and 2 weeks after treatment
- Fitzgerald skin type four or below (darker skin has risk of depigmentation).
Post-Treatment Instructions For IPL
- Sunscreen SPF 30-50 – apply every 2 hours with incidental sun exposure like walking or driving for the next two weeks
- May need soothing gel/cream/steroid cream like aloe vera gel
- Avoid picking or scratching the area of treatment
- You may have mild swelling, redness or crusting for upto 5 days after treatment
- No harsh cleansers/scrubs on your face for the next two weeks.
- You may wear makeup over the treated area if there is no broken skin
- Warm compresses to eyes for 10 min 2-3x per day for the next 3 days and then every night. (DERM mask for heat available in our office for purchase)
- It is important to take your oral omega-3s to help the glands have proper nutrition to stay healthy. Dr. Pradhan recommends the PRN brand DE3 product daily.
Schedule Your Appointment For IPL Therapy!
If you have any questions about IPL therapy and how it can treat dry eye disease, contact us at Eye Doctor MD, P.C. and a member of our staff will be happy to provide you with the information you need. To schedule an appointment with us at our local eye center, you can call us by phone at (804) 270-3333, by email at drpradhan@eyedoctormd.org, or use our online patient appointment scheduler. We have been providing the communities of Glen Allen, Richmond, and the surrounding areas with professional eye care since 2015. We look forward to helping you keep your vision clear with the quality eye care you deserve.
Watch a Video about IPL
References:
- Vegunta S, Patel D, Shen JF. Combination Therapy of Intense Pulse Light Therapy and Meibomian Gland Expession (IPL/MGX) Can Improve Dry Eye Systoms and Meibomian Gland Function in Patients with Refractory Dry Eye: A Retrospective Analysis. Cornea. 2016 Mar;35(5):318-22. doi:10.1097/ICO.0000000000000735.
- Craig JP, Chen YH, Turnbull PR. Prospective trial of intense pulsed light for the treatment of Meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2015 Feb 12;56(3):1965-70. doi:10.1167/iovs.14-15764.
- Nichols KK, Foulks GN, Bron AJ, Glasgow BJ, Dogru M, Tsubota K, Lemp MA, Sullivan DA. The international workshop on Meibomian gland dysfunction: executive summary. Invest Ophthalmol Vis Sci. 2011 Mar 30;52(4):1922-9. doi:10.1167/iovs.10-6997a.
- Toyos R, McGill, W, Briscoe D. Intense Pulsed Light Treatment for Dry Eye Disease Due to Meibomian Gland Dysfunction; A 3-Year Retrospective Study. Photomed Laser Surg. 2015 Jan 1;33(1):41-46. doi:10.1089/pho.2014.3819.
- Gupta PK, Vora GK, Matossian C, Kim M, Stinnett S. Outcomes of intense pulsed light therapy for treatment of evaporative dry eye disease. Can J Ophthalmol 2016 Aug:51(4):249-253. Doi:10.1016;j.jcjo.2016.01.005. Epub 2016 Jun 22
- Papageorgiou P, Clayton W, et al. Treatment of rosacea with intense pulsed light: Significant improvement and long-lasting results. Br J Dermatol 2008:159;3;628-632. doi: 10.1111/j.1365-2133.2008.08702.x. Epub 2008 Jun 28.
- Mark, KA, Sparacio, RM, Voigt, A, Marenus, K, Sarnoff, DS. Objective and quantitative improvement of rosacea-associated erythema after intense pulsed light treatment. Dermatol Surgery 2003;29:6:600-604.
- Clark, SM, Lanigan, SW, Marks, R. Laser treatment of erythema and telangiectasia associated with rosacea. Lasers in Medical Science 2002;17:1:26-33.
- Tan SR, Tope WD. Pulsed dye laser treatment of rosacea improves erythema, symptomatology, and quality of life. J Am Acad Dermatol 2004;51:4:592-9.
- Elmnasser N, et al. Bacterial inactivation using pulsed light. Acta Alimentaria 2007;36:3:401-408.
- Byun JY, et al. Expression of IL-10, TGF-beta(1) and TNF-alpha in cultured keratinocytes (HaCaT cells) after IPL treatment or ALA-IPL photodynamic treatment. Ann Dermatol 2009;21:1:12-7.
- Prieto VG, Sadick NS, Lloreta J, Nicholson J, Shea CR. Effects of intense pulsed light on sun-damaged human skin, routine, and ultrastructural analysis. Lasers Surg Med. 2002;30(2):82-5.